
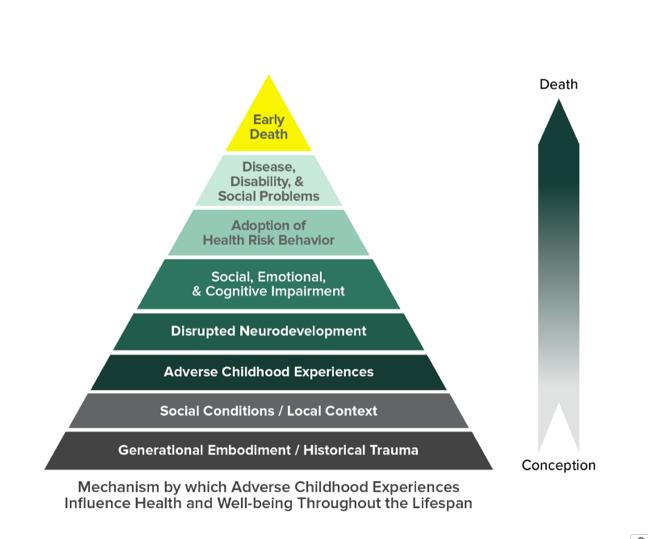
Research in Adverse Childhood Experiences (ACEs) has increased in recent years with hundreds of studies finding a strong and consistent relationship between child adversity and numerous public health outcomes (see the ACE Pyramid in Figure 1). According to the CDC, ACEs are potentially traumatic events that occur in childhood as well as the conditions in the child’s environment that can undermine their sense of safety and stability. As research on ACEs has grown, so has our thinking about how to best measure ACEs in research studies. The original ACEs studies focus on adversities in the home like abuse, neglect, and other household challenges. However, scholars agree that child adversity includes other experiences, and an expanded measure set of ACEs is needed. For example, exposure to racism (i.e., discrimination; stigma; minority stress; historical trauma) is one expanding area of research that is being considered for an “enhanced” ACE measure.
The National Survey of Children’s Health (NSCH) is a yearly nationally representative survey of children ages 0-18 in the United States that includes an ACEs question that asks parents: To the best of your knowledge, has your child ever been treated or judged unfairly because of his or her race or ethnic group?
This question attempts to measure “individual/interpersonal racism” or discrimination (per the U.S. Equal Employment Opportunity Commission: “treating someone unfavorably because he/she is of a certain race or because of personal characteristics associated with race.” According to the 2016-2018 NSCH, 10% of Black, non-Hispanic children (ages 0-18 years) have experienced individual/interpersonal racism. This equates to at least 916,803 Black children in the United States. By age, this includes about 2% of infants and 20% of teenagers. However, since this survey is reported by parents on their child’s experiences, the true rate is likely much higher. Other studies focusing in detail on perceived self-reported racism and discrimination find rates around 90% for Black children.
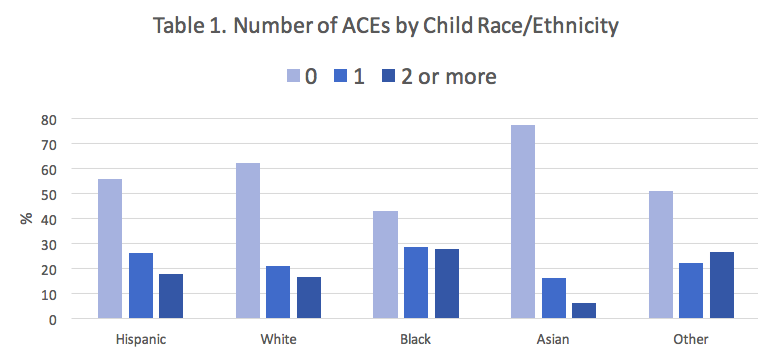
When individual/interpersonal racism is added with the 9 other ACEs measured in the NSCH to create the ACE Score, a pattern emerges comparing children in the US by race/ethnicity: Black children are more likely to have higher ACE scores compared to White children. And Black children are over-represented among children with 2 or more ACEs.
People may think, “Well, discrimination and racism are root causes of the other ACEs, such as parental incarceration, neighborhood violence, and poverty. Racism is in the groundwater of America and all negative outcomes are at least in part related to racist systems.” Yes! We see this in the ACEs data as well. Children who have experienced interpersonal discrimination are likely at higher risk for exposure to institutional/systemic racism. So, let’s see if Black children who have experienced individual discrimination have higher rates of other ACEs.
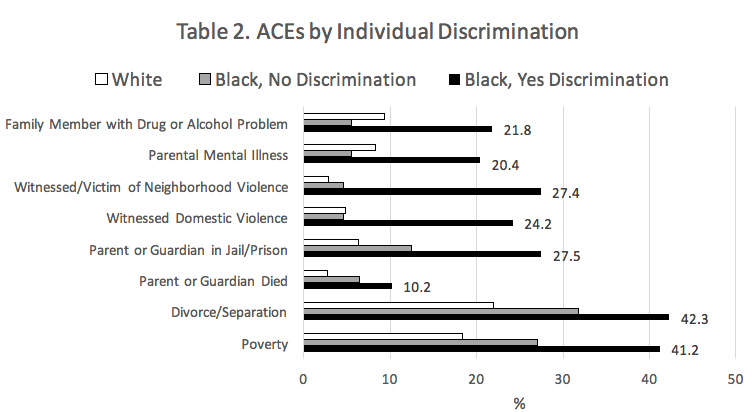
Individual/interpersonal racism is significantly associated with all other ACEs. For example, individual/interpersonal racism increases the risk (OR = 2.3) for Parent or Guardian in Jail/Prison and Witnessed/Victim of Neighborhood Violence (OR = 6.3) even after controlling for other factors.
HOWEVER: The individual/interpersonal racism measured in the NSCH is one type of racism. institutional/systemic racism are two other types of racism that exist and have been measured exhaustively in the literature.
For example, residential segregation documented among Black Americans is associated with adverse birth outcomes, increased exposure to air pollutants, shorter life span, increased risk of chronic disease, and increased rates of homicide and other crimes, adverse cardiovascular outcomes, and incidence of obesity, hypertension and nighttime ambulatory blood pressure, engagement in high-risk behaviors, alcohol use and misuse, and poor sleep. Discrimination, in and of itself, impacts individuals’ health through psychosocial stress, access to health and social resources, and violence and bodily harm, subsequently denying people of color access to resources, dignity, and a high quality of life (Davis, 2020). Research further illustrates that experiences of discrimination affect health care–seeking behaviors and adherence to medical regimens.
The NSCH measure, and all other known ACE scales, completely ignores the adverse childhood experience of living within institutional and systemic racism in America. Exposure to racism, and other ACEs, affect our health largely through the body’s stress response system. This “toxic stress” destroys critical regulation systems in our bodies and brains and can ruin our health over time. With racism on full display in the media via police killings of black people and the rise of right-wing white supremacist groups into national politics, the stress from the threat of racism is likely very high today for black children.
We believe that measures of ACEs should also include exposure to institutional/systemic racism. Why is this important for public health and social work? According to the Centers for Disease Control and Prevention (CDC), preventing ACEs could potentially reduce a large number of health conditions. For example, up to 1.9 million cases of heart disease and 21 million cases of depression could have been potentially avoided by preventing ACEs. ACEs are costly. The economic and social costs to families, communities, and society totals hundreds of billions of dollars each year. ACEs can have lasting, negative effects on health, well-being, and opportunity. Efforts to improve public health and social work services by preventing ACEs must consider how existing ACE measures ignore the true effects of institutional/systemic racism.
Data Source for Tables 1 & 2: Child and Adolescent Health Measurement Initiative (CAHMI) (2020). 2016-2018 National Survey of Children’s Health, SAS Indicator Data Set. Data Resource Center for Child and Adolescent Health supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Retrieved from childhealthdata.org.
Footnote 1: Are there other race/ethnic minority groups that experience institutional/systemic racism? Yes! We are focusing on Black children today because of the violence against Black individuals by police. Native American, Latinx, Asian, and other groups of children in America also experience the daily stress associated with minority status. Future research should explore the unique experiences of each group and subgroups.
Footnote 2: Are there other adverse childhood experiences that should be included in ACE measures? Yes! This research is underdeveloped at this point but several studies have revised and expanded the ACE measure. All other types of discrimination and stigma that children experience should be considered including classism, historical trauma, homophobia, xenophobia, sexism, transphobia, heterosexism, ableism, etc. And…there are other types of adverse childhood experiences known to create toxic stress for children including bullying, migration, war, famine, family separation, etc. that should be included in future research.
This blog post was developed in collaboration with Emma Olson, the Director of Partnerships and Evaluation with the NC Center for Health and Wellness at UNC Asheville. Several JIF students and faculty also contributed including Sarah Verbiest, Katherine Bryant, and Quinton Smith.
Additional Resources:
Hayes-Greene, Deena, and Bayard P. Love. The Groundwater Approach: Building a Practical Understanding of Structural Racism. The Racial Equity Institute. 2018. Retrieved from: https://static1.squarespace.com/static/578fa7e3d482e9af82f8f507/t/5c1b08a50ebbe8eec9f38d21/1545275564106/REI+Groundwater+Approach.pdf
Prather, Aric (2020) Stress Is A Key To Understanding Many Social Determinants Of Health. Healthy Affairs. Retrieved from: https://www.healthaffairs.org/do/10.1377/hblog20200220.839562/full/
Davis (2020) Discrimination: A Social Determinant Of Health Inequities. Health Affairs. Retrieved from: https://www.healthaffairs.org/do/10.1377/hblog20200220.518458/full/
Williams, D. R., Lawrence, J. A., & Davis, B. A. (2019). Racism and health: evidence and needed research. Annual review of public health, 40, 105-125.
Bailey, Z. D., Krieger, N., Agénor, M., Graves, J., Linos, N., & Bassett, M. T. (2017). Structural racism and health inequities in the USA: evidence and interventions. The Lancet, 389(10077), 1453-1463.
Hahn, R. A., Truman, B. I., & Williams, D. R. (2018). Civil rights as determinants of public health and racial and ethnic health equity: health care, education, employment, and housing in the United States. SSM-population health, 4, 17-24.